For clincal examples of how NPWT can bring about healing in orthopaedic situations, click here.
Potential New Treatment Modality for Treatment of Periodontal Pockets or Intraoral Wounds
Though this project started with a focus on periodontal disease, this technique might be more useful for helping intra-oral wounds to heal, and to help speed up graft incorporation.
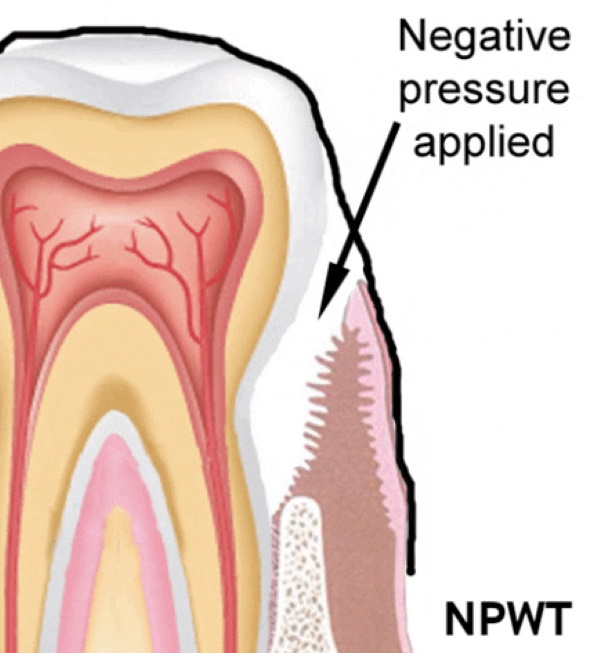
Could be useful after debridement (including cases that might involve infection) to
1) decrease edema,
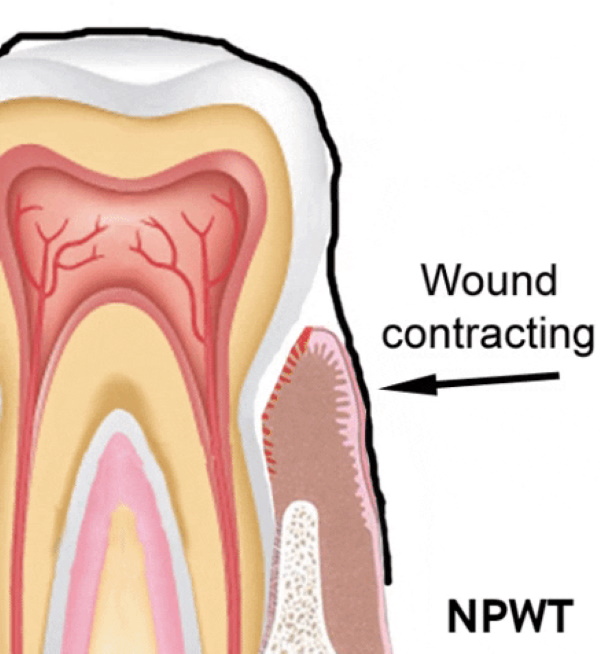
2) contract wound,
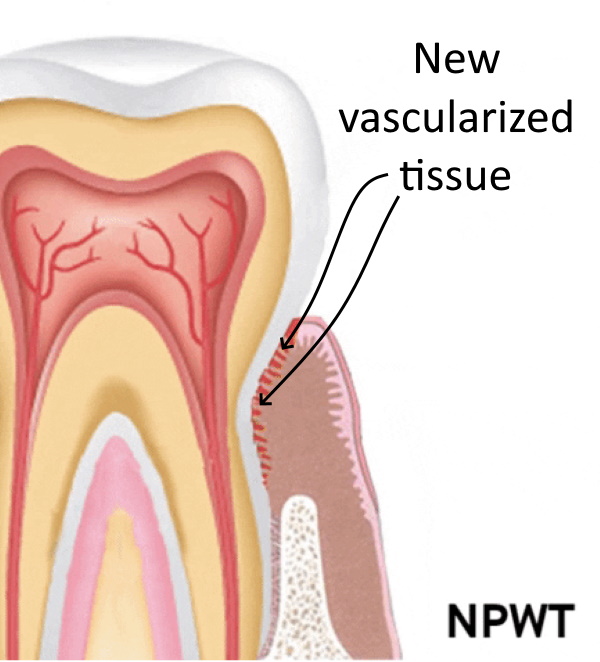
3) bring in new vascular tissue to the treated area.
Goal of this webpage: I am looking for someone to study this idea to see if it has any merit.
This idea could be a great residency research project:
--It's clinical as opposed to benchwork in a lab, and would involve little patient discomfort.
--NPWT already has proven effectiveness in orthopaedics, general surgery, and wound care.
--Simply a proof of concept would be needed to transfer this therapy to the oral environment.
--The technique incorporates treatments already invented (bleaching tray, surgical suction drain), not involving expensive technology
--This project could be relatively short.
--This adjunctive treatment in the oral space would be publishable, and would be a novel/notable project.
For a brief animation: Click here.
For more expansive video explanation: Click here.
Given the beneficial effects of NPWT as described above, here are some potential intraoral treatment scenarios:
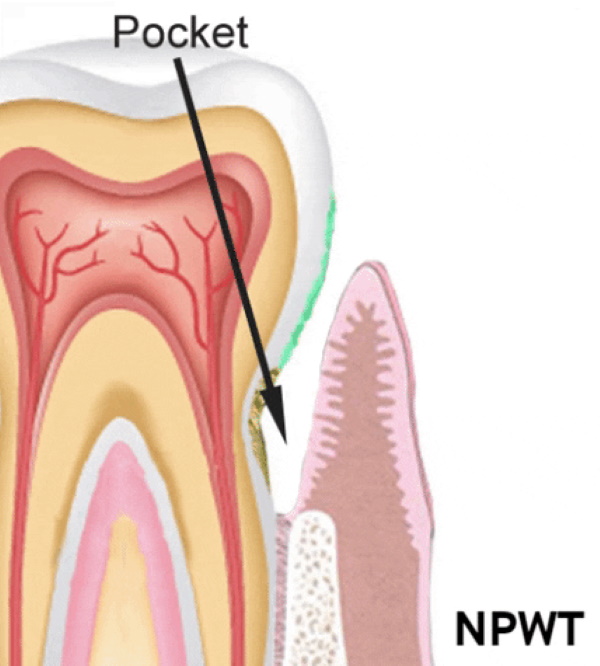
--After creating a wound by removing the gingival epithelium within the periodontal pocket, NPWT could modify the healing process to help close up the dead space (decrease pocket depth), helping with drainage also of crevicular fluid which includes tissue breakdown products. The newly vascularized tissue ingrowth could help minimize pocket depth.
--In a situation with an infected tooth or implant, after debridement, NPWT could help modulate the tissue healing and promote egress of local purulent exudates.
--In cases with multiple teeth extracted with a plan to suture soft tissue over the extraction site to prevent desiccation and prepare a bed for future grafting or implant, NPWT could decrease local edema and improve tissue health, removing exudates, and add new vascularity, optimizing tissue viability of the recipient bed, before graft or implant placement. Soft tissues would have better structural integrity and be less friable with decreased edema, and theoretic improvement of soft tissue healing.
--Similar to above, NPWT could decrease the risk of formation of a dry socket after a tooth extraction.
--In cases with osteonecrosis, after debridement of non viable bone, NPWT could hasten the vascular ingrowth to salvage as much native bone stock as possible.
Negative pressure/suction in the mouth??
If NPWT can bring about healing and salvage in challenging situations in orthopaedics and general surgery (necrotizing fasciitis cases) and with wound care, why couldn't it have an application in the oral cavity?
Could a patient tolerate having a suction tube coming out of their mouth for a prolonged period? Editorial opinion here, but when I personally had periodontal surgery, the sutures fell out at post op day 3 and tissues were largely healed. One treatment paradigm would be to apply the negative pressure for first day after debridement, removing for soft food or liquid feedings, and then for approx 12 hrs/day for next several days.
Bacteriology:
NPWT is applied irrespective of the bacterial flora. When wound vac (NPWT) dressings are changed in the orthopaedic setting, there is no pretense or expectation of sterility, as with the improved microvascular environment, tissue growth and healing occurs.
Probably in the mouth, as elsewhere in the body, once the regenerative tissue forms, there is a soft tissue remodeling process, creating structurally stable tissues.
For a video about an alternative oral appliance idea, to apply negative pressure without having to take an impression of the patient's teeth (about 3 minutes long): click here.
Assuming that his idea has merit, though I currently lack clinical data (orthopedists don't work in the mouth), I tried to outline a paper for a potential case report: click here.
How to apply negative pressure?
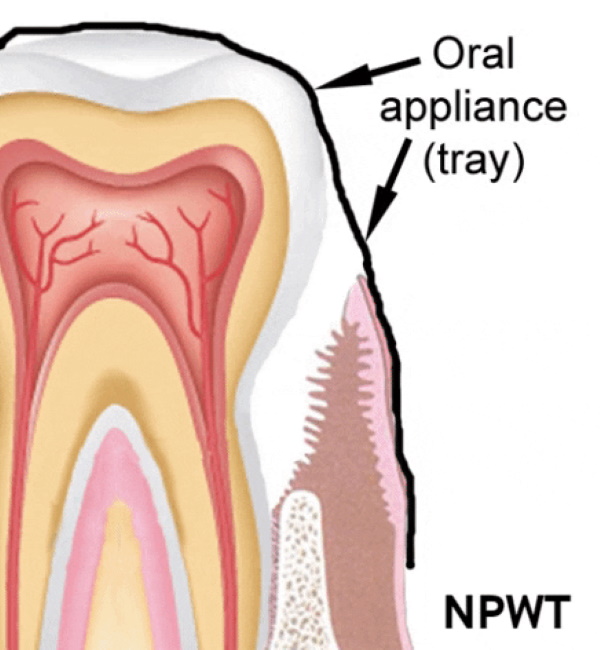
Whereas in the spine and extremities, there is need for some type of adhesive dressing and a sponge to distribute the negative pressure over the wound surface, some anatomic details of the mouth, with moist mucosa, and spaces between the teeth, are favorable to the application of negative pressure. Ideally, the appliance that would apply negative pressure would be like a thin flexible bleaching tray that extends to contact the gingival tissues, made of supple material, and could be fabricated with a channel near the gingival sulcus to both direct the negative pressure to the gum-tooth interface, and also allow for easy application and removal of the appliance (other details noted in my 11 minute video). Certainly, there are those in the oral health fields that have more access that I did to form the appropriate appliance.
An oral appliance prototype (right) was designed that was comfortable to wear (personal experience), and the treatment would be needed on only a short term basis. The negative pressure was applied by attaching the concave surface (surface facing teeth and gums) to a surgical suction drain. The sealing to prevent a leak was optimized with a small amount of a dental adhesive (like Poligrip) to the region in contact with the hard palate.
Since my 11 minute video referenced above was made, I have learned that it might be possible to make a model of the patient’s dentition and soft tissues using information from a 3D image source, like CT scan, and CADCAM technology, although making a dental impression would probably be less expensive.
However, with ideas outlined in another short video here, I show how it might be possible to apply the negative pressure without having to make a model of the patient's dentition.

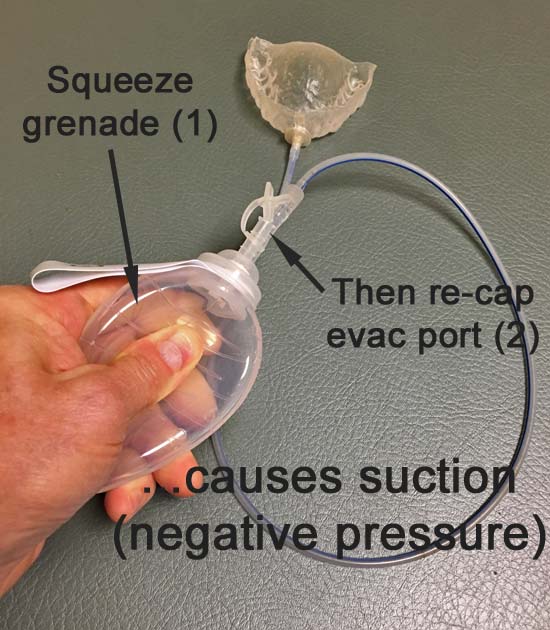
Negative pressure can be generated with a powered pump, but I was able to generate negative pressure with a surgical suction drain as pictured here on left.
The suction from the concave aspect of the appliance was enough to keep the appliance attached to the treatment surface (teeth and gingiva) without requiring the need for the patient to have any muscular effort from the tongue to keep the appliance in place.
The appliance stays in place like a suction cup would stay stuck to a smooth surface.
While in the spine and extremities, the negative pressure is maintained using an adherent dressing creating a seal on the surrounding skin, the moist surfaces in the mouth would not require adhesives to make a seal as long as the appliance fit the patient's anatomy and was relatively compliant.
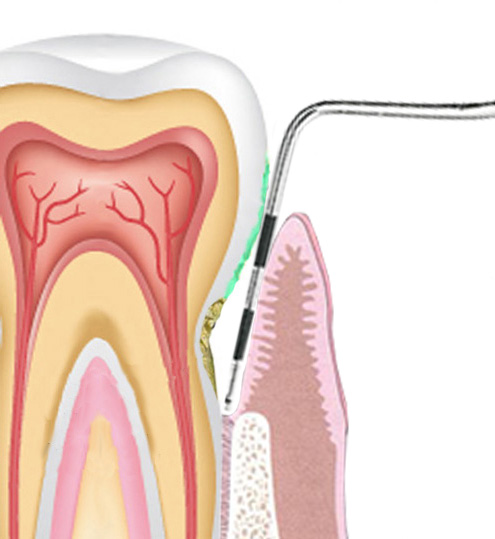
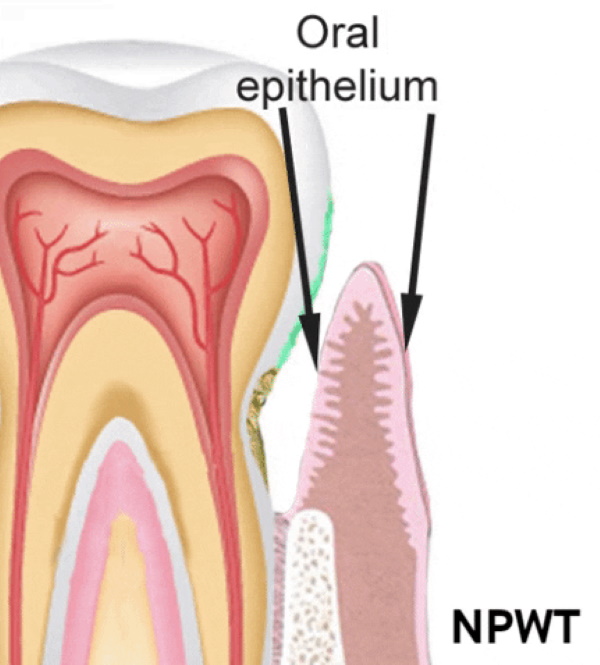
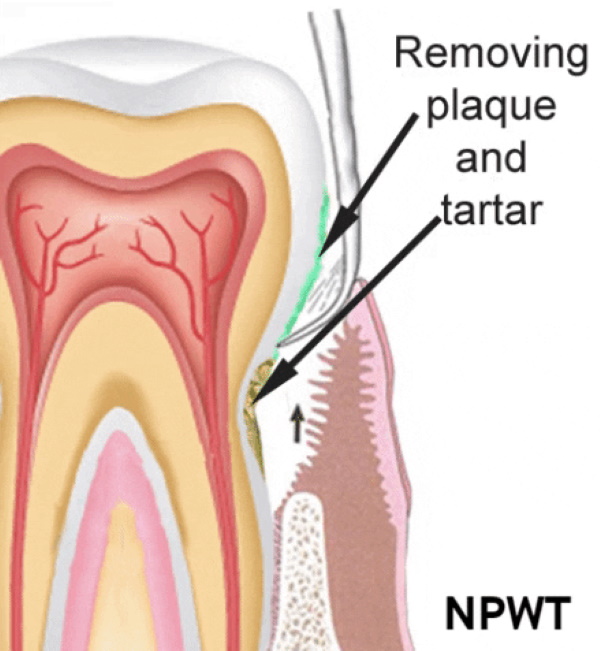
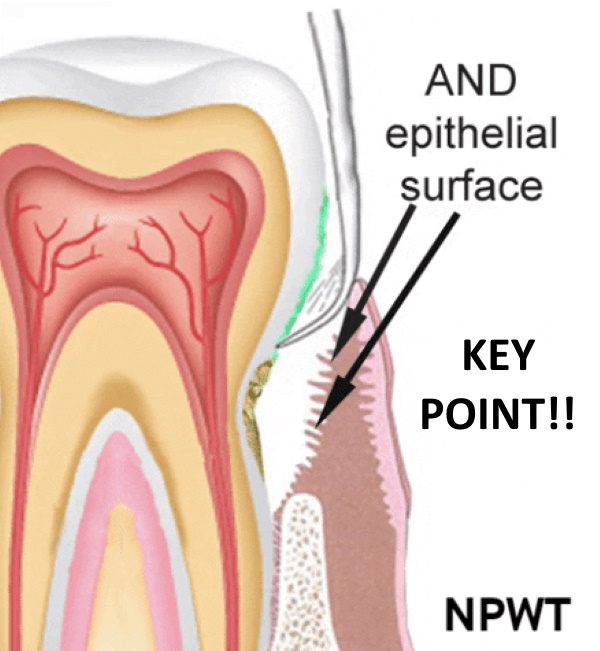
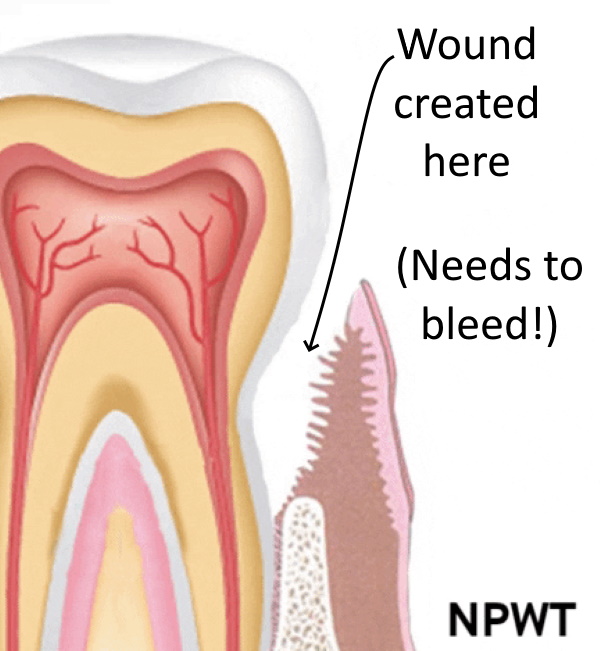
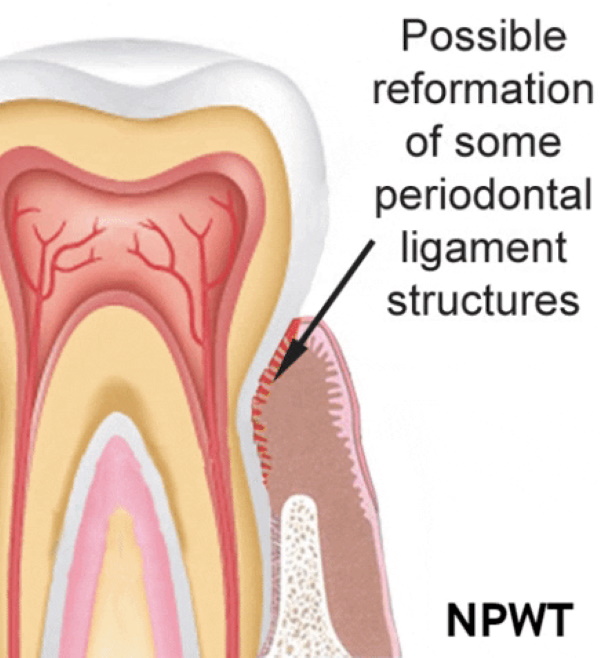
As a potential modality to bring about decreased depth for treatment of periodonal pockets, shown in the illustrations below, simply the application of negative pressure by itself would not bring about healing after debridement to cause decreased pocket depth.
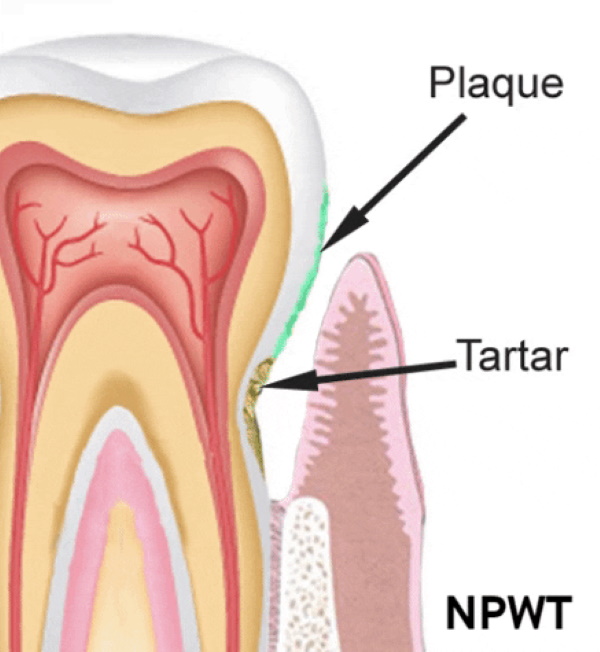
The deepest parts of the pockets would have to be cleaned, tartar and plaque removed, but more importantly, the surface layer of the oral epithelium lining the pocket would have to be removed creating a wound, with bleeding tissue, for any tissue reattachment to occur.
If no wound is created (if it's not bleeding with a healing process initiated), there is no process for NPWT to affect.
Below is a photo of NPWT being applied to a dorsal foot wound through application of a sponge to distribute negative pressure to the wound surface.


Thoughts on potential study design:
When I returned to my periodontist, he noted that at one week, there was still inflammation, so the process could have been applied for longer than 36 hrs.
Possible treatment plan: wear the appliance as much as possible for the first 24 hrs, and then 12 hrs a day (patients could wear at home and at night) for next 7-10 days.
