An intermediate step, after medications and physical therapy, and before surgery, is an epidural injection.
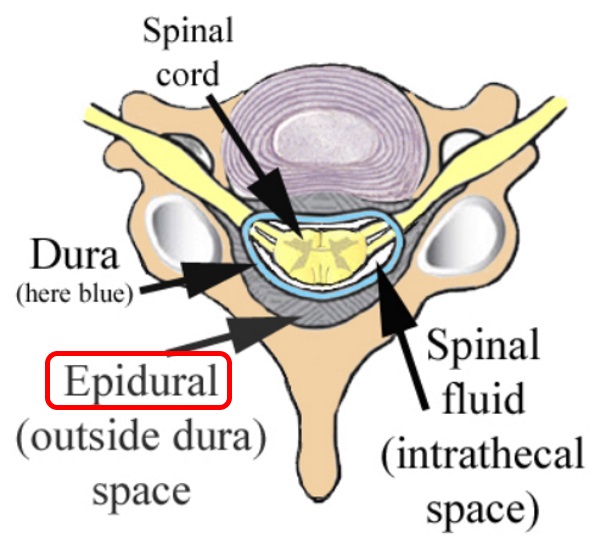
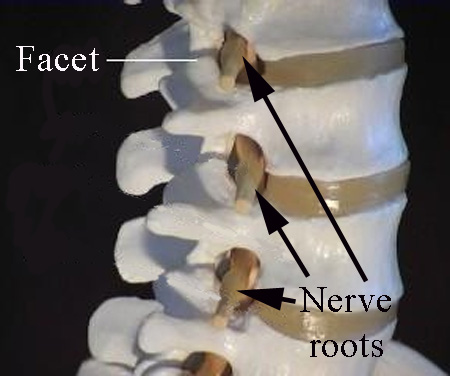
The dura is the tissue that keeps the spinal fluid around the spinal cord and spinal nerves. This diagram to the right which is from the cervical (neck) region shows the spinal cord, but in the lumbar spine, since the spinal cord ends about the L1 vertebra, the area within the dura is filled with nerve roots.
With regard to the terminology, the prefix “epi” refers to the space outside of, so the word “epidural” refers to the space outside of the dura.
The idea is to inject medication, usually some form of cortisone and some local anesthetic, into this space to calm down pain and inflammation affecting the nerves and nerve roots.
For a discussion of the risks, click here.
With xray guidance, a needle can be introduced into this space to administer steroid medications (usually some form of cortisone) to calm down pain associated with these nerve roots.
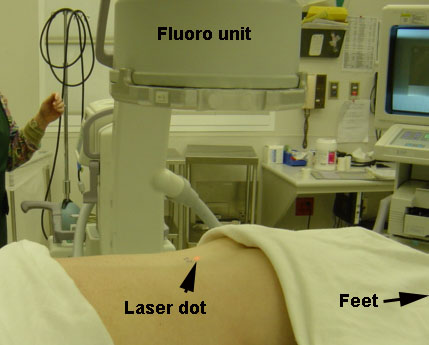
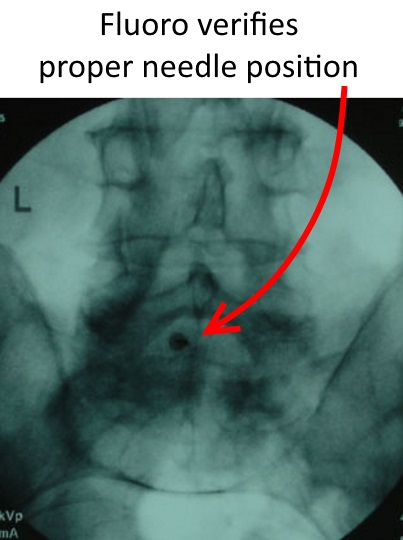
This injection is done in the operating room with some sedation, and X-ray is used to be sure the needle is introduced into the right space. Usually the patient, although sedated, is still awake, so that the doctor can be informed in there is any unexpected pain, as might occur (happens rarely) if the needle tip touches the nerve.
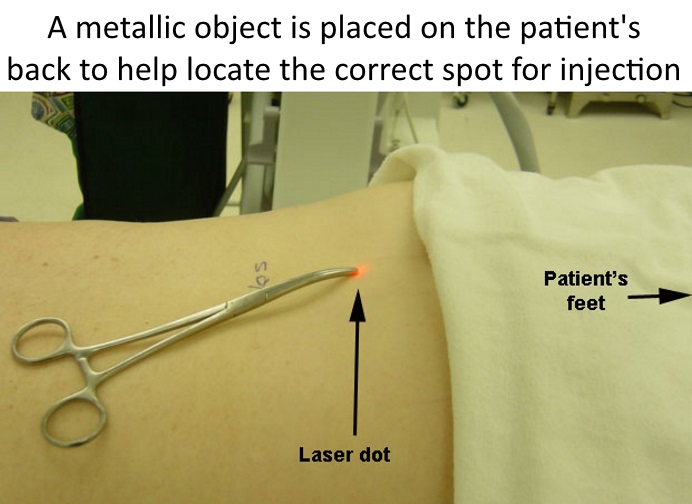
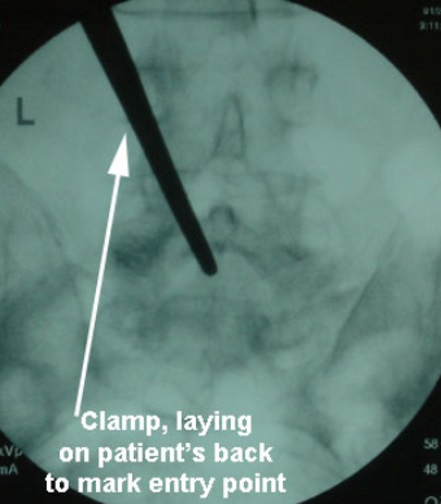
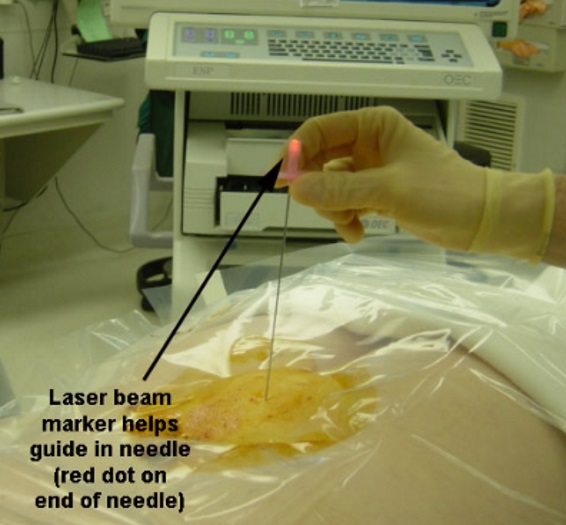
The point of the needle is where the laser dot was shining on the skin. By aligning the other end of the needle also with the dot, the path or direction of the needle to go perfectly aligned into the right disc space is much easier to achieve than without the laser guidance, especially in larger patients (below left). The needle in the interspace (at the right level) can be confirmed on fluoro, which is a live action portable X-ray (below right).
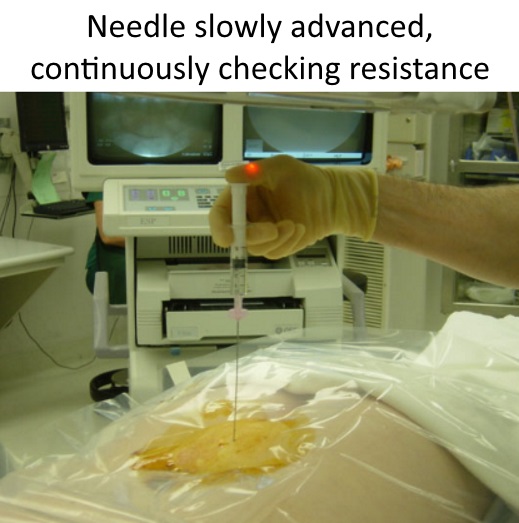
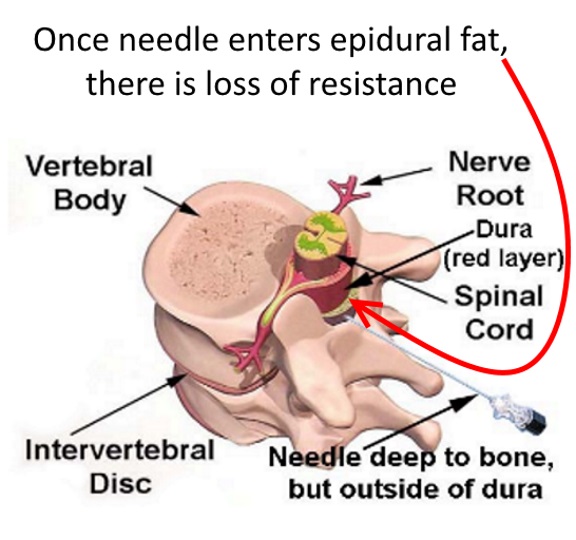
Once the needle barely passes through the ligament (thick soft tissue), there is a loss of resistance. The needle is aspirated (sucked back) to be sure no spinal fluid is withdrawn.


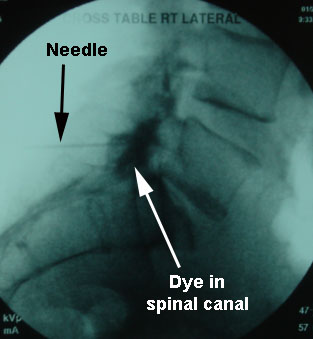
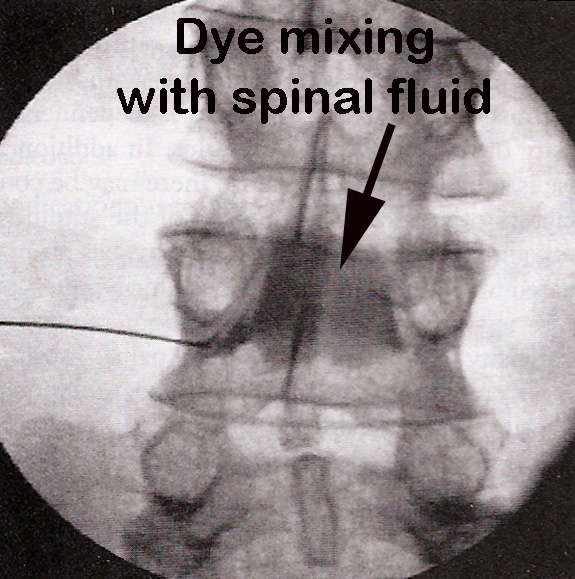
The dye is placed through the needle to be sure the needle tip is in the spinal canal (where the nerves are).
The dye can be seen on this lateral (side) view.

On this frontal view, the dye can be seen in the midline, where the spinal canal is.
Once the needle tip is confirmed in the right place, and no spinal fluid is retrieved with backward sucking on the syringe, the medications for the epidural injection are injected, usually including some combination of a cortisone preparation and some numbing medicine.
Transforaminal Injection:
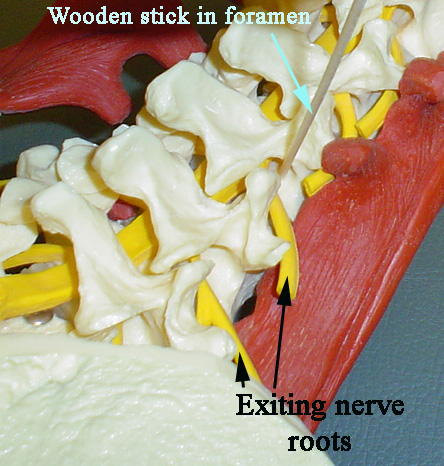
Another type of injection is through the foramen, which is the opening on the side of the spine through which, at each level, a nerve exits.
This injection, called transforaminal, is done by directing the needle closer to the nerve root that exits through the foramen.
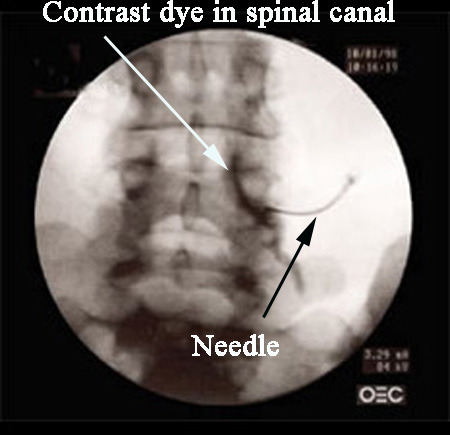
As seen in this xray image, the needle directs the contrast dye both along the nerve root, and into the spinal canal, where the rest of the nerves and the neighboring disc are located.
Since this injection goes closer to the nerve root, it has to be done with the patient awake to let the doctor know if there is pain down the leg with needle insertion. If this pain does, occur, the needle is backed up immediately.
Here is an example of what we don’t want to achieve with a foraminal injection (this picture from a textbook!) where the needle was placed within the nerve root, and the contrast dye can be seen spreading into the space occupied by the spinal fluid (intrathecal injection).
Usually, there are two different medications mixed in the same syringe:
numbing medicine (lidocaine or marcaine), for some immediate relief, and
steroid (like cortisone), for longer lasting and sustained relief.
Sometimes, patients will feel better the first day (from the numbing), and then a little worse (numbing worn off), then start to feel better again (cortisone starting), with hopefully a long lasting effect.
