I've had it with Ambetter. Ambetter is a super low quality insurance product.
For link to a brief youtube video on this topic, click here. Though they can't seem to approve an MRI, they can sponsor NASCAR.
As a healthcare provider in Georgia, I take care of many patients with Ambetter (parent company Centene) "insurance." Based on mounting frustrations with this insurer, I need to share my impressions/opinions:
-->The word "insurance" is not representative, implying that the insurer will cover the insured (the patient) for, in this case, health care costs. However, instead of covering these costs so that patients can have a reasonable expectation of receiving healthcare with their health insurance, I see insurers (like Ambetter/Centene here) denying almost everything I recommend.
-->Their sin of omission is that they neglect to inform their customers that the way they can provide their "low cost" product is that they in fact cover very little of what we doctors recommend
-->As illustrated below, the fact that their denials harm patients apparently has little influence over their efforts to deny care.
-->They hide their denial process behind opaque/unclear guidelines to deny care, and the denial letters give either no reason, or a vague and irrelevant reason for the denial of care.
-->As with anyone behaving in an inappropriate fashion, they will never admit to their incentives.
-->You have to watch what they do, not what they say. The way they roll, I would be strongly surprised if any Ambetter executives have Ambetter insurance.
-->As illustrated below, my perception is that they are clearly acting in bad faith, even though they have outsourced the job of being the bad guy to another company called Turning Point.
-->They routinely mislead and fail to provide care to the citizens of Georgia who are least able to fight for themselves to receive appropriate evaluation and treatment in a timely fashion.
-->The denials are made by people who will never see or examine the patient, and more often than not, providers in a different specialty (why should I be talking with an OB doctor about a spine case?)
--> I know of no provider or patient in the Albany, GA area who is happy with the Ambetter insurance product. Other docs have described Ambetter denying essential labs, and even antibiotics in the setting of an infection, forcing patients to pay for these items out of pocket even though the patients supposedly have "insurance."
-->They never offer an alternative treatment plan
-->It's nearly impossible to get a human on the phone to discuss any issues
Ambetter obstructs (or has obstructed) access to care on every level.
EXAMPLE CASE: For pt DB, who has given me permission to share her story: Since Ambetter/Turning Point behavior is beyond explanation, I need to publicize their bad behavior, along with copies of formal complaints I have made.
Details of the case:
--The patient was clearly getting worse, with spinal cord compression that would not improve without surgery.
--Despite having had three requests for surgery, and even a peer to peer conversation with another spine surgeon who verbally approved the case, surgery was still denied. Though with Herculean efforts the surgery was eventually approved, my staff and myself spent easily greater than SIX hours on battling the process of approval: This type of delay and obstruction is beyond acceptable and is not a sustainable provider/insurer relationship.
--Surgery was requested when she had coverage mid December '22, but then without explanation, Ambetter cancelled her policy on 1/2/23. DB notes she was not informed of this cancellation, though somehow her policy was reinstated Feb '23. Is an insurer generated lapse in coverage acceptable?
--The denial letters from their utilization review company Turning Point offer no explanation as to reasons for the denial.
There is no planet on which treating my patient this way would be acceptable.
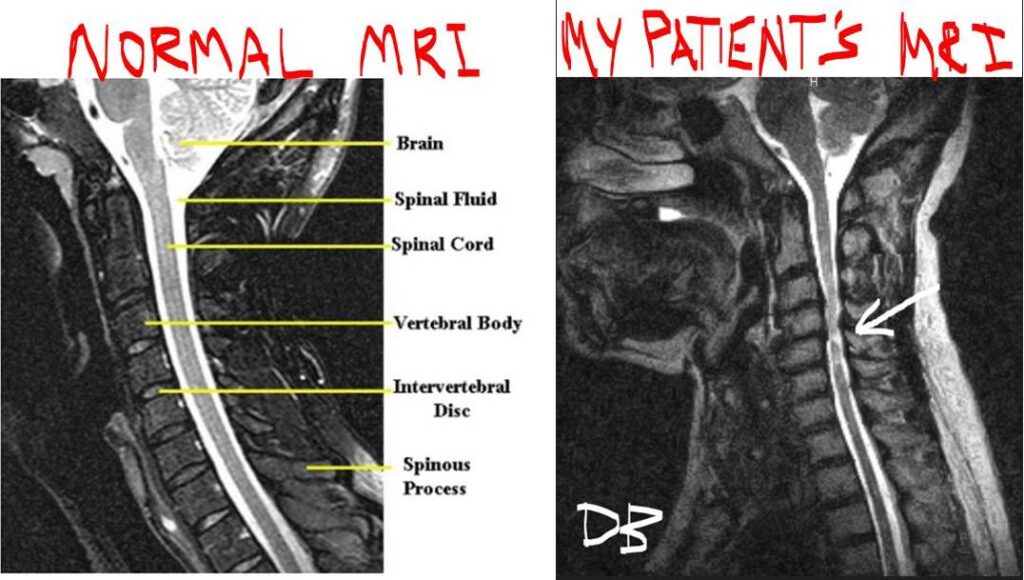
Comparing here a normal and my patient's cervical spine MRI, I think a six year old could tell that, for my patient, something isn't right. Her spinal cord is compressed, and she can barely walk. There was no way short of surgery to help this patient, but her treatment was denied multiple times for no comprehensible reason, with approval efforts requiring multiple appeals. I even had to Tweet at the company (see below) to get anyone's attention. My opinion is that the way this patient was handled is not only inappropriate and unacceptable, but likely represents a clinical decision making system that inherently act is BAD FAITH.
After becoming exhausted about the continued denials, with almost no response on several cases, I went on Twitter and surprisingly, I had a tweet back to me in TEN MINUTES that someone would get back to me
Is this the new world order, that I have to go on social media to get a response from an insurance company?
My protest
efforts -->

--> I made a complaint against Ambetter that they were acting in bad faith, with the complaint sent to: Ambetter, Peach State Health Plan, GA Insurance Commissioner, Medical Association of GA, Atlanta Journal Constitution, with copy to DB (the patient). To see a copy, click here.
--> Here are the THREE denials for care in this case DB above, with no explanation as to why or what additional information might be needed, even after my peer to peer review with a spine surgeon where he agreed with the plan. For the letter dated 1/3/23 (on second page), it is unclear even if the surgery is approved or not, but the cover letter said the service request had been denied. We requested peer to peer, but no call for three days. We had to spend many hours trying to fight for approval. To see the documents, click here.
--> DB's surgery was requested in Dec '22, and Ambetter cancelled her insurance in Jan '23 with no reason indicated. DB was not informed of this cancellation. To see the document, click here (though policy re-started in Feb '23).
--> I made a complaint to National Committee on Quality Assurance, an organization that is supposed to assure quality for healthplans that can be seen by clicking here.
--> By the way, Ambetter goes to great lengths to obstruct providers from being able to deliver care. For Ambetter to avoid any responsibility for the denials of care, Ambetter has subcontracted with another company called Turning Point to determine if any requested procedures can be approved. Turning Point's criteria for deciding what is appropriate care, despite the shiny happy faces on their website, by being almost impossible to achieve, gives them plenty of leeway to deny almost any request (Dear Patient, the service requested by your doctor is "not medically necessary."). Click here.
--> Having received a response from the National Committee on Quality Assurrance indicating no interest from their Customer Support Manager indicating no actual interest in "quality assurance," I wrote to their board of directors so at least they can be informed of how quality is not being assured. To see my letter, click here.
Responses -->

--> Response to me from the GA Insurance Commissioner. Bottom line: They are doing nothing. To see the correspondence, click here.
--> I responded to their response, noting that they did not address my complaint. To see this letter, click here.
--> The National Committee on Quality Assurance (NCQA) response to my complaint, in my opinion, was very weak. To see it, click here.
--> I responded back to NCQA noting that for an organization that has "quality assurance" right in their name, there wasn't much quality assurance going on. To see the letter, click here.
--> Medical Director Dr. James Richardson responded to me about my NCQA complaint along with my response to them, still not addressing my issues, can be seen if you click here.
--> Ambetter (through their contracted company Turning Point), in my experience, is mostly obstructive to the delivery of patient care for patients who have this insurance product. However, Ambetter, while not explaining their denials nor the criteria they use to determine what is appropriate care, still has enough money left over to sponsor NASCAR (see left).
--> I made a complaint to the Office of the GA Governor, who forward the complaint to GA Dept of Community Health...no response.
BOTTOM LINE: Who is helping patients in this regard? My opinion: Nobody!!
I think the only strategy is for patients, if they have an option for choosing an insurance product, to know is the "quality" (if that word is applicable here) of the product they are buying.
ANOTHER EXAMPLE CASE: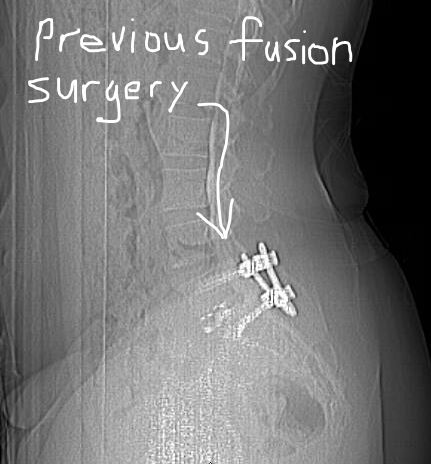 This case involves another patient, TS.
This case involves another patient, TS.
TS had previous fusion surgery at L5S1. This surgery, a minimally invasive lumbar fusion, illustrated in these three web pages (page 1, page 2, and page 3), was supposed to bring about a bony connection between the L5 and S1 vertebral bodies (bones fused together), but in a minority of cases, this surgical goal is not achieved.
In TS's case, the bone did not grow to connect the two vertebral bodies.
TS had improvement initially after the surgery, but since the fusion did not occur, she had began several months after the surgery to have more pain that gradually increased. Not wanting to have another surgery, she waited and hoped for improvment, tried physical therapy, activity modification, different pain medicines, but with gradually worsening symptoms, decided to proceed with further work up (tests/evaluation).
We were able to get a test called a CT myelogram (pictured on right), where the radiologists inject contrast dye into the spinal fluid and then they get a lumbar CT scan. This study confirmed the cause of the patient's worsening pain: no bone growth in the space between the vertebral bodies. The patient weighed her options both for and against a revision surgery, understanding the risks, and that the only guarantee is that there is no guarantee. She elected to proceed.
The surgery was first partly approved by Ambetter and then within a day, denied completely. As you will note in the submitted paperwork (click here), no comprehensible reason is offered. The records were submitted as they requested.
Clearly, the only interest of Ambetter is not in helping TS get better, but saving money.
If Ambetter/Turning Point recognized that surgeons look at images (CT myelograms) themselves in pre op planning and don't rely on reports of radiologists who will never see the patient, they would have noted the nonunion (but they didn't).
If Ambetter/Turning Point needed additional info specifically, they could have specified such (but they didn't).
If Ambetter/Turning Point had an ounce of compassion, they could have suggested an alternative treatment (but they didn't).
Addendum: 3/31/23: We did get approval for the TS surgery, but the process was still inappropriate, and onerous, and opaque. My criticisms still stand that it was unclear what additional information was needed to get approval for the surgery, and I see no evidence of improvement of this process.
For the record, if Ambetter wanted to actually take care of patients, I would be glad to comply with their guidelines.
I would be glad to deliver appropriate care, and to follow guidelines that are reasonable. However, I cannot find their guidelines on their websites, and they certainly don't share what the issues were in their denial letters. If they at least brought some clarity about why my requests for evaluation or treatments were denied, I could supply the needed information and learn to do so for future requests, and then I could take care of the patients in our community. Apparently, however, actually helping patients is bad for the Ambetter/Centene business model.
It would be more honest if maybe they changed their name to AmWorse. Then, when the patient comes to the doctor, who orders a medication or treatment, we providers in the room, along with the patient seeking care, could at least realize, "Oh yeah, what was I thinking? Of course I shouldn't expect to be taken care of. I have AmWorse!!"
Though this assessment is morbid humor, I have yet to find one patient with Ambetter coverage who would disagree with this characterization of the care available, or more accurately, not available, with this "insurance" product.
Maybe the folks at Ambetter are in the teaching business, and they are teaching me/us a lesson for having tried to work with them.
From a pure money making standpoint, Ambetter's behavior actually makes total sense when you think about the business model of insurance. The company collects money (premiums) for the promise of covering medical expenses for their customers. However, these medical expenses, when approved, are their expenditures. More revenue and less expense means more profit for the company. Basic. Approving more patient care means more expense (less profit). Therefore, they are highly incentivized to be as obstructive as possible to authorize any expenditures that might be significant.
The insurance carriers, who have de facto control of essentially all of medical care, cannot be held liable for their actions, and they will never meet the patients to know if their actions cause more harm and suffering. Their priority is to maintain the next quarter's profits to please their shareholders. Oh, and apparently to sponsor NASCAR events.
I am quite sure that companies like Ambetter and Centene approached lawmakers in various states with the promise of managing their medicaid expenditures (a promise attractive to legislators), but leave out the detail that the "managing" means withholding care. And of course, how do I know whether these managed care corporations take their profits off the top, leaving even less money for delivery of care??
In my entire career, I have never had an insurer suggest another treatment plan. Their most powerul words are essential telling providers to take a hike. Approvals are less common, but they are certainly fluent with the terms "denied." and "not medically necessary."
In a recent article I noted about another insurance company Cigna, this type of insurer behavior is not limited to Ambetter: Link here.
My personal experience here as a provider:
Ambetter denies nearly everything. Consumers should beware of this small (and undisclosed) detail.
Other examples:
There will be many examples and I will be glad to add them to this page:
-->MRI denied: Understanding that there are criteria that have to be met to approve imaging studies, this patient, Mr. MS, had all the symptoms of and the physical exam findings to strongly suggest a herniated disc with severe back pain, pain down the leg, and had failed conservative treatment for over a year. He had undergone physical therapy, including a home program, various medicines, epidural injections (in other words, all the boxes were checked), and we got a notice that the MRI request was judged as "not medically necessary," with no other explanation. The denial was signed by an OB-GYN physician (so, should I be reviewing his reasons for doing hysterectomies??)
My assistant called to set up a peer to peer review, and sat on hold for 30 minutes. Wait, let me rephrase that: THIRTY MINUTES!!!!
until I was able to speak with the physician reviewer, who also is not a spine surgeon, who noted that the reason for the denial was that my office note did not specify the exact dates that the patient had undergone physical therapy treatments. Are you kidding me?? What's next? Do I need to specify the temperature of the hot towels used on his back? Is there a doctor looking at these issues? Does anyone there get the big picture of what is happening with my patient? Or...is the system designed to obstruct approval of anything that could cost a dollar?? (Ed. opinion: seems that way to me. Just as no person trying to manipulate a system would ever admit it, we have to look at what they do, not what they say).
The denial letter said nothing of this secret criteria (needing exact dates), and for that thirty minutes on hold, my assistant was not able to do any other of her duties in our office. And what if a patient couldn't afford the co-pay for their physical therapy, or got worse with therapy, or had transportation issues: Sorry, no MRI for you!
Maybe I'm the one that's slow to learn, but at least Ambetter's outgoing message would be more honest if it said, "Thank you calling Ambetter. Please hold for your turn to talk to the hand."
-->Approval for surgery: My partner who does sports medicine had a 14 yr old patient with a torn anterior cruciate ligament, a major ligament in the knee and who needs surgery to be able to participate in sports in the future. Although he had represented to the grandmother (has custody) that surgery has risks, that there is no guarantee, along with the anticipated post op course, the surgery was denied (found out later after again being on hold for a prolonged period), that the reason for denial was that the individual risks were not specifically named. The documentation said only that the requested procedure was "not medically necessary" which is insurance-speak for "go jump in a lake," and our scheduler learned about the reason for denial only in a phone call. Another sentence was subsequently added to the medical note with the specific words detailing the risks that had already been discussed, and though the surgery was requested in November '22, it finally was approved for mid Feb '23. Was this delay necessary?
My assessment of the new world order in healthcare (as it has been for several years now):
Your doctor is not actually your doctor.
The insurance company, who will never meet or examine you, is your doctor.
Which states have Ambetter?
Any reviews?
Apparently, Ambetter is in multiple states, and based on this website I found, I am not alone in my impressions.

