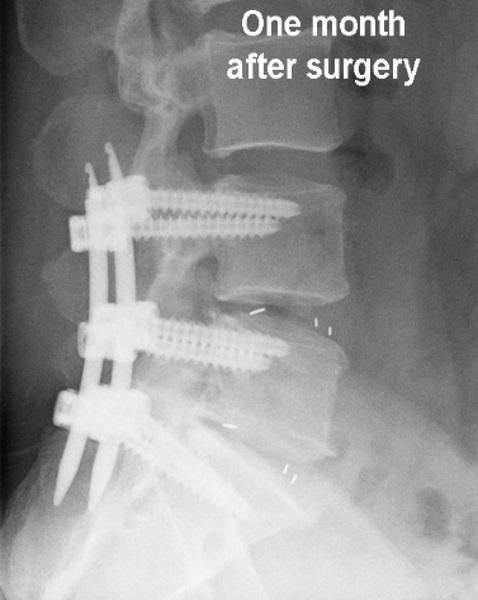
A spinal fusion is an operation to create an environment to cause two or more spinal bones (vertebrae) to grow together into one, thereby eliminating the pain caused by the arthritis or instability of the spine. The fusion is usually done by removing the soft tissue between the bones (disc between the vertebral bodies) and creating a biologic situation where, like fracture healing, additional bone grows in the area being fused.


vs.
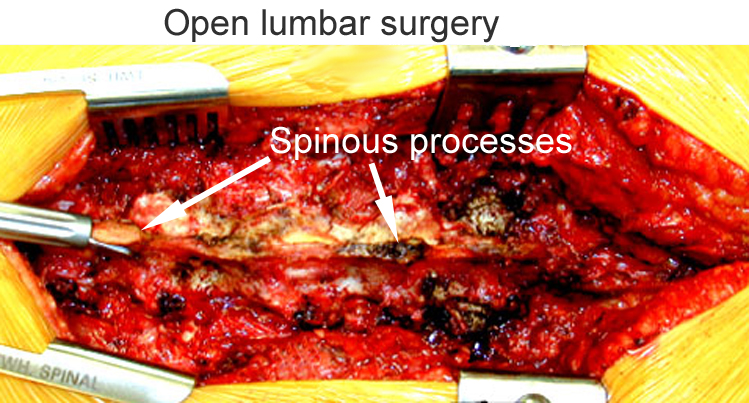
An open approach is pictured here above right for comparison. While open surgery looks severe, this approach is very common. At the end of the surgery, the wound is sutured closed, however, the muscles are stretched open by the retractors, often for several hours, during the case. There are many situations where an open approach is required.
With a minimally invasive approach using the tubular retractor system, there is less pressure on the surrounding muscles. The surrounding muscles are exposed to less pressure from the retractors, and wind up less bruised. The surgical wound is smaller and therefore has less surface area exposed to the environment of the operating room. Less muscle is dissected off the bone, thus preserving the blood supply to the spinal bones. Due to these factors, there may be at least a theoretical decreased risk of infection with minimally invasive cases. Click here for more info on minimally invasive approach.
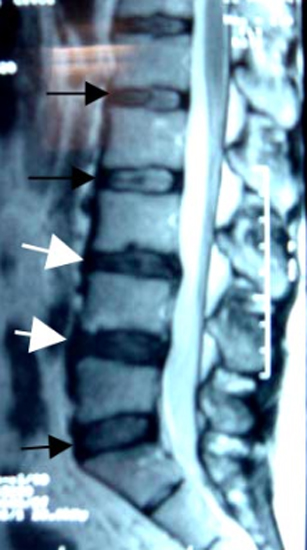
Example case
Here is an example case of a patient who needed a two level fusion. The normal discs are indicated with the black arrows, and the white arrows are pointing to the damaged discs. Note they lack the white center of the other discs. In this MRI imaging sequence, water shows up white, and in the damaged discs, the center (jelly in the donut) is dried out, which is one of the signs of damage.
This patient, who had primarily unremitting low back pain, also failed to improve with non-operative treatment.
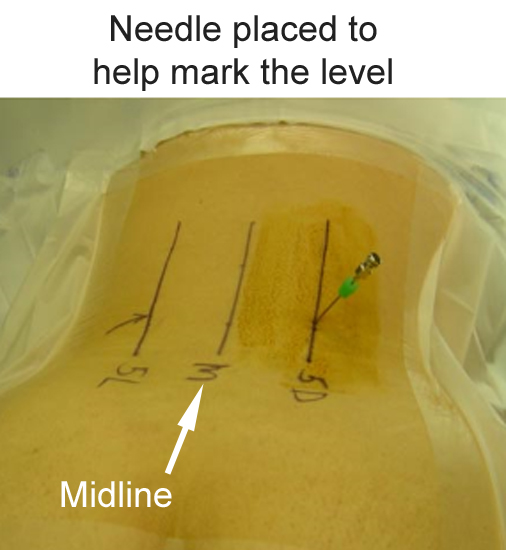
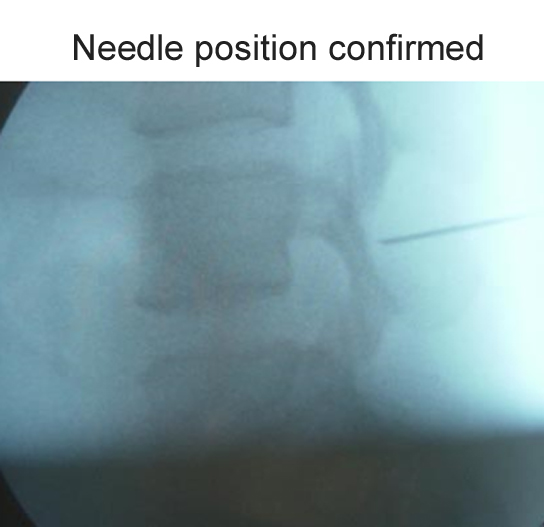
The patient is positioned on the operating table face down. With fluoroscopy (X-ray), we can see the levels of the spine. After sterile prep and drape of the low back, a needle is placed with position confirmed with fluoro to be the correct level. This step is very important as the spinal bones look the same.
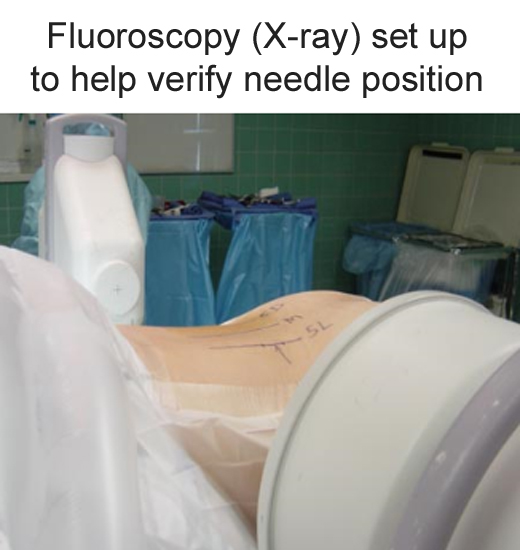
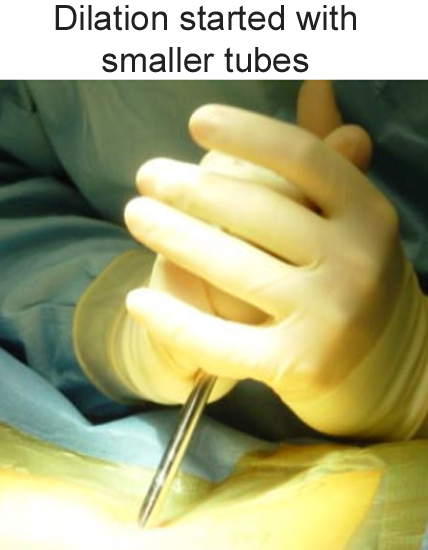
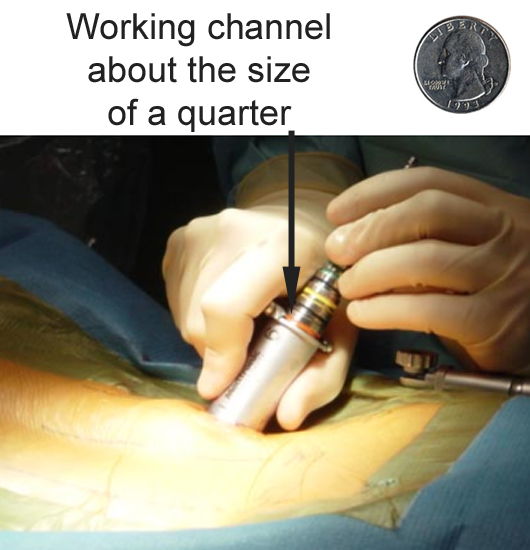
A small incision is made, and the dilation of the working pathway starts with small tubular retractors (with placement guided with fluoro) with further dilation up to larger tubes.

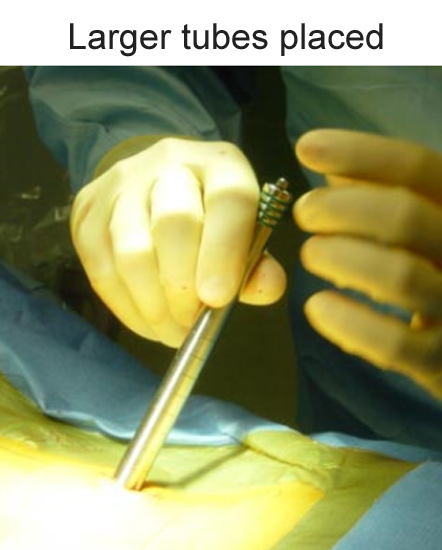
The dilation continues until we have the final tubular retractor in place that is 26 mm in diameter, or about the size of a quarter. Position is again confirmed fluoroscopically.


As will be detailed on the following pages
Min Invasive Lumbar Fusion, page 2
Min Invasive Lumbar Fusion, page 3
the surgery can be done through this tubular retractor with assistance of an operating microscope and further imaging with fluoroscopy, without having to make a large incision.

